Table of Contents
Background
Sexual health, as defined by the World Health Organization (WHO), is a “state of physical, emotional, mental and social wellbeing related to sexuality; not merely the absence of dysfunction or infirmity.”1 Sexuality, an expression of our sexual health, is an inherently human trait and a basic human right that applies to all individuals. Unfortunately, female sexual health is an area in medicine that is frequently dismissed and often overlooked due its complexity and multifactorial nature. Additional barriers exist for aging women to access information and professional help regarding sexuality, resulting in inadequate treatment. Unfortunately, these barriers frequently involve inadequacy on the part of healthcare providers, including lack of time during the clinic visit, lack of sexual education, lack of confidence in one’s own ability to diagnose and treat, worry about causing offense in addressing sexual health concerns, in addition to personal discomfort among providers.2 Moreover, it takes a multidisciplinary team and further medical training to address a multitude of symptoms and concerns while providing comprehensive evaluation and care.
Sexual concerns and symptoms worsen during midlife. Midlife is the stage in a woman’s life when dynamic changes in sex steroid hormones (estrogen, progesterone, and testosterone) occur leading to a complete cessation of their production by the ovaries once a woman reaches menopause. Sex steroids play a major role in positively regulating sexual behavior, mood, emotion, and cognition throughout a woman’s lifespan. Declining levels of sex steroids during perimenopause, and extremely low levels in postmenopause, are associated with deleterious consequences on overall health and sexual well-being. It is understood from the Study of Women’s Health Across the Nation (SWAN) and others that sexual function declines with advancing menopause status and begins in the menopausal transition or perimenopause, including in women who have hysterectomies.3 The most frequently reported concerns related to sexual health at midlife include low sexual desire (40–55%), poor lubrication (25–30%) and dyspareunia (12–45%), one of the complications of genitourinary syndrome of menopause (GSM).2 These concerns cause sexual dysfunction (SD) at this time in a woman’s life that stem from deeply-rooted factors, including biological, psychological, emotional, and socio-cultural origin and thus, a biopsychosocial assessment must be performed. In this section, the focus will be on the biological factors and hormonal influences.
The association between androgen levels and sexual function
It is worth noting that sexual dysfunction is more than just related to estrogen deficiency, which has always been an area of focus in earlier studies in menopause and sexual function. However, estrogen and androgen have been found to have a synergistic relationship and stimulatory effect on the female sexual response, promoting sexual desire on the brain reward systems through a complex network of neurotransmitters and dopaminergic pathways involving excitatory and inhibitory signals.4 Recent preclinical and clinical molecular studies have identified androgen’s pivotal role as a regulatory hormone of female sexual function. Androgen or testosterone decline, as it relates to sexual dysfunction, is due to natural aging and is independent of menopause. The production of testosterone’s precursor hormone, dehydroepiandrosterone (DHEA), by the adrenal glands progressively declines as one ages. But, despite a high production of DHEA in the ovaries, DHEA is not able to prevent the sexual dysfunction concerns that affect women. Young women who have undergone removal of both ovaries surgically, causing surgical menopause, have double the risk of developing low sexual desire compared to women with natural menopause.5 This change is explained by the abrupt decrease in serum testosterone levels observed in young women since bilateral oophorectomy or surgical removal of both ovaries is associated with lower total and free testosterone levels than natural menopause. Thus, the type of menopause plays a role in sexual dysfunction, but no serum testosterone concentration correlates with the presence or absence of low sexual desire or its severity. Furthermore, sexual function is inversely correlated with the severity of menopausal symptoms such as vasomotor symptoms (hot flashes, night sweats), which is commonly understood among healthcare providers providing menopausal care and is widely supported in the research literature.6
Is there a role for testosterone therapy in women?
The role of testosterone in the management of low sexual desire is not completely understood but research and clinical evidence support a beneficial effect of testosterone therapy on sexual desire when premenopausal physiologic levels of testosterone are maintained. According to the Global Consensus Position Statement on the Use of Testosterone Therapy for Women, testosterone therapy is recommended for treatment of low sexual desire or Hypoactive Sexual Desire Disorder (HSDD) in postmenopausal women after a full biopsychosocial assessment has been performed and other conditions, such as dyspareunia or pain with intercourse, fatigue secondary to vasomotor symptoms, anemia, thyroid disease, anxiety and depression, medication side effects, and relationship issues, that contribute to low desire are concurrently addressed including.7 Candidates for testosterone therapy are postmenopausal women presenting with a decline in sexual interest with or without diminished arousal that causes sufficient personal or interpersonal concern (distress).7 Women who are deemed not good candidates for testosterone therapy are those with signs of clinical hyperandrogenism or androgen excess (i.e., acne, hirsutism, voice deepening, androgenic alopecia) or are using an antiandrogenic medication (i.e., finasteride, dutasteride).7 Testosterone therapy for women with a history of hormone-dependent neoplasia should only be recommended in consultation with the woman’s oncology team providing cancer care.7
Vulvovaginal changes with normal aging and Genitourinary Syndrome of Menopause (GSM)
Women experience vulvovaginal changes with age due to decreasing collagen production and loss of elasticity and moisture, influenced by loss of sex steroids. The vulva and vagina house both estrogen and androgen receptors and with the decline of these hormones, atrophy and inflammation of the vulvovaginal tissues result. Women experience changes in the vulva including thinning and paleness of the labia majora and minora, narrowing of the introital opening and vaginal canal, graying of pubic hair, and loss of lubrication. There may also be a decline in blood flow to the clitoris, causing it to be less sensitive to touch and stimulation leading to decreased sensation and arousal. Pelvic floor muscles that support the uterus also weaken as women age and may cause less intense and pleasurable contractions, leading to decreased orgasms.
It is worth noting that it is not just the vulvovaginal tissues that are affected by the decline in sex steroids but also the urethra and the bladder, causing concerns related to Genitourinary Syndrome of Menopause (GSM). GSM, previously referred to as vulvovaginal atrophy, encompasses the vulvar, vaginal, urethral and bladder symptoms that affect ~27%-84% of postmenopausal women.8 The urethra and vestibule can also exhibit pallor and thinness with overlying erythematous blood vessels owing to thinning of the mucosa surrounding these areas.8 Outgrowth of the urethral meatus, also known as a caruncle, is a commonly seen lesion with GSM.8 The inner vaginal mucosa loses its folds called rugae and becomes pale and increasingly friable and thin. These changes result in painful pelvic exams, pain with vaginal penetration, dysuria, frequent urinary tract infections (UTIs), and discomfort with activities of daily living.
Treatments for Genitourinary Syndrome of Menopause (GSM)
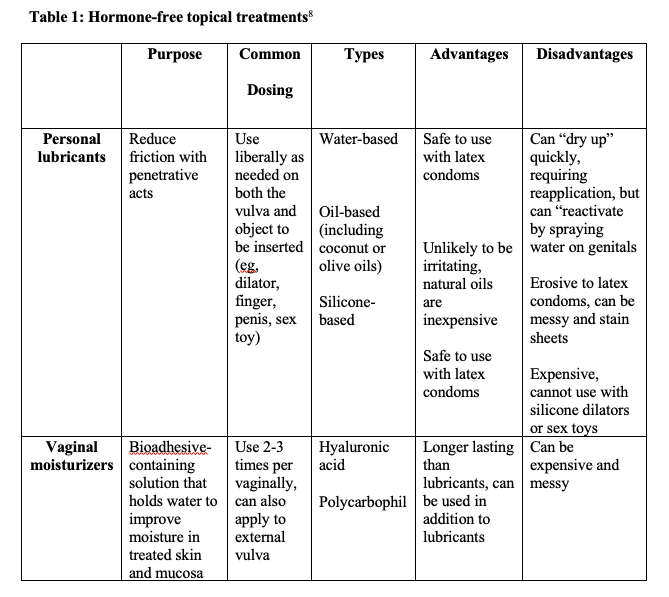
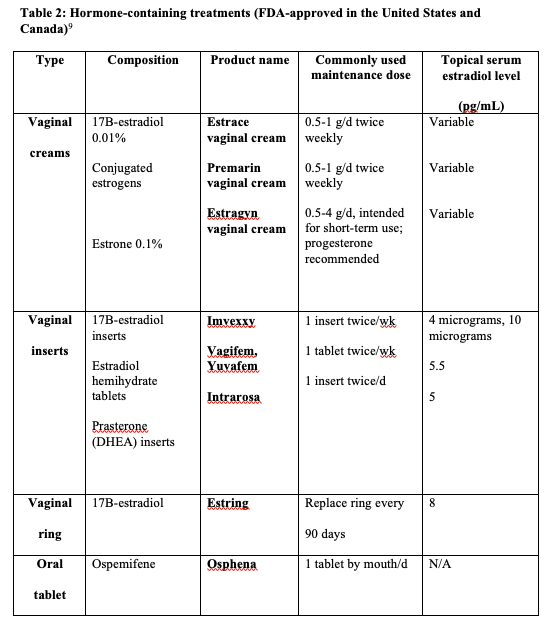
There are a variety of treatments for GSM that can be categorized as non-hormonal and hormonal. Please see Tables 1 and 2 for a detailed description of each option. Treatment options depend on a woman’s health history, personal risk factors, and preferences. This care involves an individualized approach and a discussion that prioritizes shared decision making.
Conclusion
Healthcare providers play valuable roles in addressing and managing sexual health concerns among midlife women. There are many safe and effective treatment options to manage the biological and hormonal factors that cause sexual dysfunction in women. The choice of formulation must be individualized after thoroughly assessing a woman’s concerns, health, medical history, preferences, and treatment goals. Engaging a woman in healthcare decision-making is warranted to improve sexual health outcomes that will improve patient sexual satisfaction and quality of life at midlife and beyond.
References
- WHO. Defining Sexual Health: Report of a Technical Consultation on Sexual Health. Geneva; 2002.
- Scavello I, Maseroli E, Stasi V, Vignozzi L. Sexual Health in Menopause. 2019;55(9):559. doi:10.3390/medicina55090559
- Avis NE, Colvin A, Karlamangla AS, et al. Change in sexual functioning over the menopausal transition: results from the Study of Women’s Health Across the Nation. Menopause. 2017;24(4):379-390. doi:10.1097/GME.0000000000000770
- Tobiansky DJ, Wallin-Miller KG, Floresco SB, Wood RI, Soma KK. Androgen Regulation of the Mesocorticolimbic System and Executive Function. Frontiers in endocrinology. 2018;9:279. doi:10.3389/fendo.2018.00279
- Kokcu A, Kurtoglu E, Bildircin D, Celik H, Kaya A, Alper T. Does surgical menopause affect sexual performance differently from natural menopause? The journal of sexual medicine. 2015;12(6):1407-1414. doi:10.1111/jsm.12891
- Nazarpour S, Simbar M, Tehrani FR. Factors affecting sexual function in menopause: A review article. Taiwanese journal of obstetrics & gynecology. 2016;55(4):480-487. doi:10.1016/j.tjog.2016.06.001
- Parish SJ, Simon JA, Davis SR, et al. International Society for the Study of Women’s Sexual Health Clinical Practice Guideline for the Use of Systemic Testosterone for Hypoactive Sexual Desire Disorder in Women. The journal of sexual medicine. 2021;18(5):849-867. doi:10.1016/j.jsxm.2020.10.009
- Hoeppner CG, Cigna ST, Perkins J, Gaba ND. Sexual Health. Clinics in geriatric medicine. 2021;37(4):553-577. doi:10.1016/j.cger.2021.05.004
- The NAMS. GSM Position Statement Editorial Panel. Menopause. 2020;27(9):976-992. doi:10.1097/GME.0000000000001609
Citation
Moreno C. (2024). Understanding Menopause and Sexual Function from the Biological and Hormonal Perspective. Utah Women’s Health Review.

